Add Your Heading Text Here
One of the greatest benefits of transitioning TPN from the hospital to home TPN is that patients gain the autonomy to manage their condition comfortably at home rather than in a hospital or clinical setting.
Not only can this help TPN patients return to some of their normal routines, but home TPN has been reported to help some patients achieve better clinical outcomes with care in the comfort of their own homes.
When first starting out, patients and caregivers transitioning from hospital TPN to home TPN sometimes face uncertainty as they shift to a new way of life. Things like learning how to set up TPN at home and finding a comfortable rhythm with the daily administration of your nutrition are some of the biggest challenges they may face.
With the right education and support, these challenges can be overcome as patients make the transition from hospital to home while receiving TPN. In this blog, we’ll address some of the most common issues and questions patients have when they are first getting started on home TPN.
How Does Home TPN Differ from TPN in the Hospital?
The setting is the primary differentiator between receiving home TPN vs. hospital TPN care – and that is a good thing!
In a hospital setting, patients will be attended to by healthcare professionals, such as nurses, doctors, and pharmacists, in a clinical environment where they will be closely monitored to ensure they receive the correct amount of nutrients and that no complications develop.
Home TPN allows patients to receive their therapy in a more comfortable environment. The patient or a caregiver is responsible for TPN administration, including organizing supplies and preparing the medication for infusion.
How is TPN Delivered to a Patient’s Home?
While the process can vary, going home with TPN generally includes the following steps:
- The hospital care team will coordinate the medical and care needs to prepare a patient to receive home TPN including:
- Finalize a home TPN prescription. A physician will prescribe a TPN formulation to meet a patient’s nutritional needs.
- Provide options for selecting a home infusion pharmacy. Patients have the right to select their home TPN provider. While patients may receive a referral from their physician, it’s helpful to keep their options open until they find a provider capable of meeting their lifestyle and preferred standard of care.
- Work with the Home TPN provider to order your TPN and supplies. Once patients have selected their home TPN provider, they will begin ordering their medication and supplies. The home TPN provider will arrange shipping and establish a delivery schedule so patients will always receive their medication on time.
- Receive your home TPN formulation and supplies. The home TPN provider will carefully ship patients their formulation in temperature-controlled packaging so the medication remains safe to use upon arrival. Patients should contact their provider if their medication arrives late or is damaged.
How to Store Home TPN Formula Bags at Home?
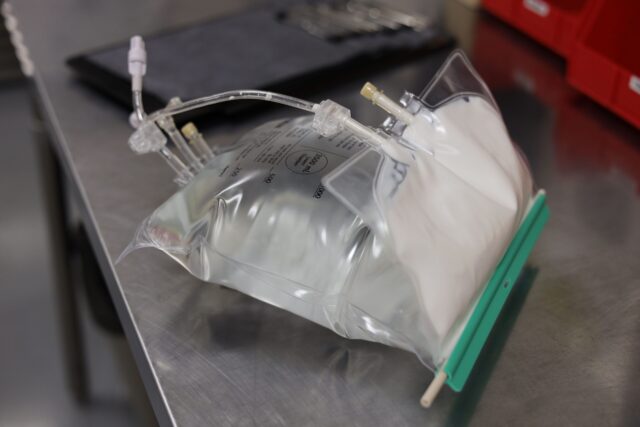
Home TPN formula requires refrigeration when not in use. However, storing home TPN and hydration bags in your refrigerator can be problematic. Home TPN bags can occupy a lot of space in a refrigerator, and some patients don’t feel comfortable storing medicine and food in such proximity.
Using a separate refrigerator to store TPN frees up space in the family refrigerator and eliminates the uncomfortable factor of keeping food and medicine together. In addition, with a separate refrigerator, patients can keep their TPN bags near the rest of their home TPN supplies and equipment for more convenient access.
How to Prepare Home TPN Formula for Use?
Before starting home TPN for the day, it is recommended that patients remove the formula bag from the refrigerator and allow it to come to room temperature. This usually takes one or two hours, or possibly more, depending on the temperature of the patient’s home. Patients should avoid placing the TPN in direct sunlight or around pets when bringing their medication to room temperature.
What temperature TPN should be when starting is a matter of preference. Some patients are more sensitive to cold than others, while others prefer to receive their TPN at a colder temperature.
The temperature at which TPN is administered makes no difference to its efficacy, but some patients find it uncomfortable to receive their formulation when cold. However, remember that when administering TPN, the formula will warm up a little as it moves through the central line of the pump.
How Can Patients Lower Their Risk of Infection?
Home TPN patients have an increased risk of infection due to using an intravenous catheter. Fortunately, there are several steps patients can take to lower their risk of infection.
Practice strict hygiene
Thorough hand washing before and after handling TPN supplies will lower infection risk.
Maintain a clean household
Keeping a home clean and clutter-free will help avoid exposing TPN supplies to contaminants.
Follow proper catheter care procedures
Patients must ensure their catheter insertion site remains clean and adequately dressed while following their healthcare provider’s recommended schedule for catheter changes.
Monitor for signs of an infection
Watching for signs of infection, such as redness, fever, or swelling, at the catheter site will inform patients whether they need to contact their healthcare provider for assistance.
When is Home TPN Used for Patients?
When a patient is healthy enough to leave the hospital but still requires nutritional support, home TPN offers a solution that allows them to live a healthy and active life. Patients on home TPN need to receive thorough training and educational support on administering their formulation and may require the assistance of a nurse or caregiver during the infusion process. But living on home TPN is manageable and offers an improved quality of life compared to hospital TPN.
Transitioning to home TPN can feel overwhelming, but patients have support options to guide them through the uncertainty of managing their nutritional care. Their doctors, nurses, friends, family, and home infusion providers can all assist in providing the emotional and informational support patients require to successfully transition TPN into part of their daily lives.
Additional Resources for Patients and Doctors
For patients just starting their home TPN journeys, or doctors looking to provide their patients with additional resources, download our Checklist for Starting TPN, which includes useful information and helpful tips for starting TPN at home.
Home TPN is a journey, but never a journey a patient should have to go alone.
Got questions? We’re here to help. Contact a home TPN specialist at Nutrishare today, or explore our Nutrishare Neighborhood – a free resource center for home TPN patients, their family and friends and clinicians alike.
Frequently Asked Questions
How does home TPN differ from hospital TPN?
In a hospital setting, patients are attended to by healthcare professionals in a clinical environment, while home TPN allows patients to receive their therapy in a more comfortable environment, with the patient or a caregiver responsible for TPN administration.
How is TPN delivered to a patient’s home?
The hospital care team will coordinate the medical and care needs to prepare a patient to receive home TPN, including finalizing a home TPN prescription, providing options for selecting a home infusion pharmacy, and working with the home TPN provider to order the TPN and supplies.
How can patients lower their risk of infection while on home TPN?
Patients can lower their risk of infection by practicing strict hygiene, maintaining a clean household, following proper catheter care procedures, and monitoring for signs of infection.
When is home TPN used for patients?
Home TPN is used when a patient is healthy enough to leave the hospital but still requires nutritional support, and they need to receive thorough training and educational support on administering their formulation.